Hospital News
-

What Your Annual Blood Work Can Reveal About Your Health
December 22, 2025Your yearly blood work gives your provider information they can’t see during a physical exam, sometimes before you notice any symptoms at all. Blood work isn’t only for sick visits – routine lab work plays a key role in preventive care and long-term health. In Las Cruces, New Mexico, many…
Learn more -

Employee Spotlight: 'I Carry My Culture With Pride'
November 26, 2025At Memorial Medical Center, we are proud to celebrate the rich histories, living traditions, and enduring contributions of Native people during Native American Heritage Month. Today, we honor one of our own, Shannon Toledo, a valued member of our Health Information Management team whose journey, culture, and spirit bring warmth and meaning to our…
Learn more -
.jpg)
Is It a Cold, the Flu, or Something Else? How to Tell the Difference
November 25, 2025When your child starts coughing, sneezing, or running a fever, it can be hard to know what you’re dealing with. As the seasons change and kids head back to school or daycare, coughs and sniffles start making the rounds. Here in Las Cruces, NM, that often leaves parents asking: is it just a cold, or something more serious like the flu, RSV, or…
Learn more -

Employee Spotlight: ‘NICU Is What I Love To Do’
November 20, 2025For Lisa Hernandez, NICU nursing is a career calling very close to her heart.
Learn more -

Understanding and Preventing Diabetes
November 14, 2025The first step in preventing diabetes is knowing your risk. A simple blood sugar test can determine if you have diabetes or prediabetes.
Learn more -
Memorial Minute: October 27, 2025
October 27, 2025News from the leadership team at Memorial Medical Center.
Learn more -

Safely Manage Medications to Protect Your Personal and Community Health
October 22, 2025While medications can play a vital role in healing and managing health conditions, they can also pose serious risks when misused.
Learn more -
MMC Invites Community To Annual Public Board Meeting On November 13th
October 21, 2025This meeting will feature a short presentation on hospital updates as well as a Q&A and interactive session with attendees.
Learn more -
.jpg)
What Does Breast Cancer Look Like in Its Early Stages?
October 21, 2025Breast cancer is one of the most common cancers in women, and early detection can dramatically improve outcomes. But what does breast cancer actually look like in its earliest stages? It’s not always a visible lump – early signs can be subtle, and knowing what to watch for can make all the difference. Below are some common early signs and symptoms to be…
Learn more -

MMC Now Offering Genetic Testing For Hereditary Cancer At Women's Imaging Center
October 08, 2025To empower and inform patients who have a personal and/or family history of cancer, Memorial Medical Center is now offering a hereditary cancer risk assessment and genetic testing to qualifying individuals during their routine mammogram screening.
Learn more -

Why You Shouldn’t Skip Your Annual Physical: Screenings That Save Lives
September 26, 2025Many people put off their annual physical, if they feel fine, there’s no urgent need to visit the doctor. But skipping your yearly check-up can mean missing the early signs of serious conditions that are often treatable if caught early. At Memorial Medical Center, we believe prevention is just as important as treatment. Your annual physical is a chance to…
Learn more -

Employee Spotlight: Marcie Fredericksen Inducted Into Las Cruces Bowling Hall Of Fame
September 19, 2025MMC is proud to celebrate one of our own, Marcie Fredericksen, who was recently introduced as the newest member of the Las Cruces United States Bowling Congress (USBC) Hall of Fame 2025. Marcie has been an avid bowler for over the last 30 years, earning countless accomplishments along the way. She was named the 2019 Women’s Bowler of the Year and finished second in…
Learn more -

Memorial Medical Center Receives Chest Pain Center Reaccreditation
September 18, 2025Hospital continues to provide necessary care, resources to patients with heart attack symptoms
Learn more -
Memorial Minute: September 8, 2025
September 08, 2025News from the leadership team at Memorial Medical Center.
Learn more -

How to Protect Your Child from Fall Viruses like Flu, RSV, and COVID
September 03, 2025In warmer parts of the country like Las Cruces, NM, respiratory virus season can begin as early as September and stretch well into the winter. With kids back in school, viruses like flu, RSV, and COVID-19 start spreading quickly – especially among young children whose immune systems are still developing. As a parent, you can take steps now to help protect…
Learn more -

Memorial Medical Center Launches Program to Improve Maternal Health and Save Lives in Our Community
August 29, 2025This innovative program provides postpartum patients with wristbands to wear for six weeks after delivery, helping ensure they receive timely and appropriate care for any potential complications.
Learn more -
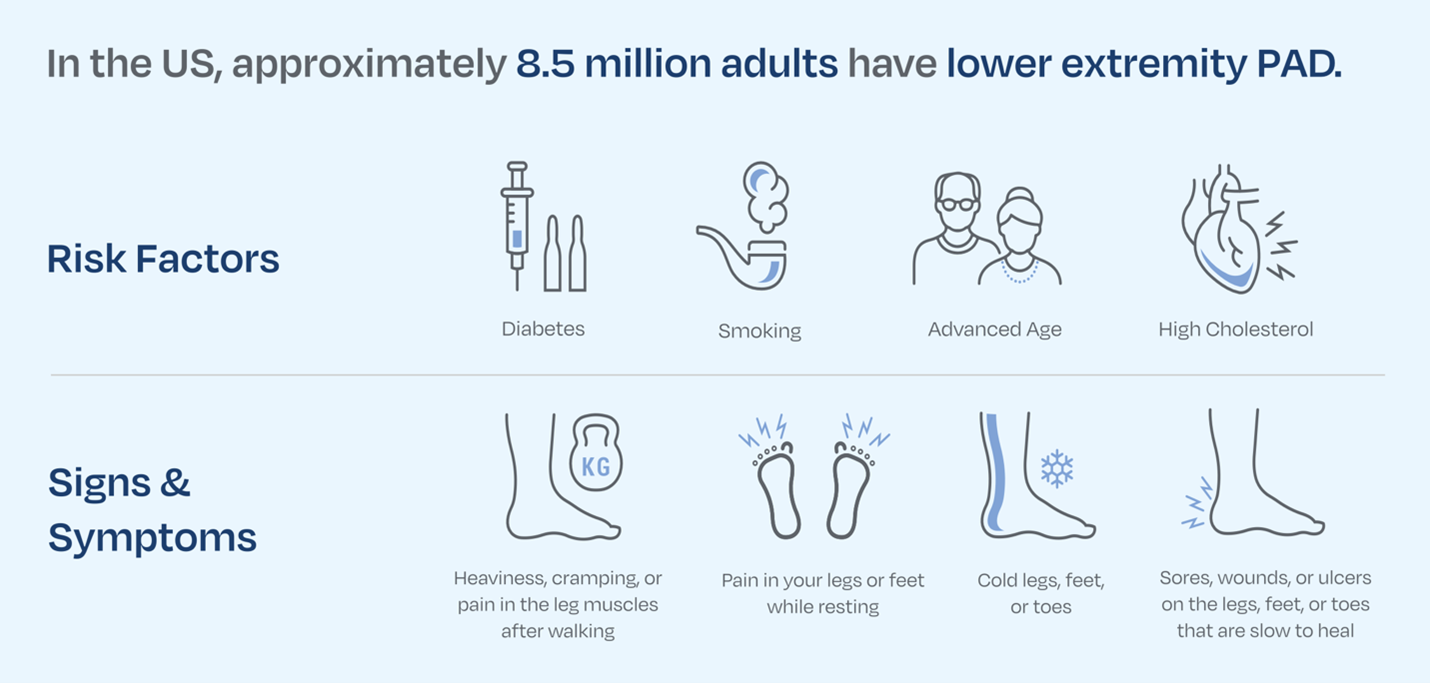
In Regional First, Memorial Offers Cutting-Edge Procedure For Complex PAD
August 27, 2025Udit Bhatnagar, MD, FACC, FSCAI, RPVI, is the first in our region to treat complex PAD using an innovative new therapy called Percutaneous Transmural Arterial Bypass.
Learn more -

MMC Now Offering Minimally Invasive Solution For Those Suffering From Chronic Tendon Pain
August 13, 2025Dr. Matthew Endrizzi is the only provider in Southern New Mexico and El Paso offering new treatment for conditions like tennis elbow, plantar fasciitis and Achilles tendinitis
Learn more -
.jpg)
Why Mosquito-Borne Illnesses Are on the Rise — and How to Protect Yourself
August 01, 2025Warmer weather and standing water are fueling a surge in mosquito-borne diseases. Here’s what you need to know and how to prevent them.
Learn more -
Memorial Minute: July 31st, 2025
August 01, 2025News from the leadership team at Memorial Medical Center.
Learn more
